Since the SARS-CoV-2 variant known as B.1.617 was first reported in India late last year, it has spread to dozens of other countries — including the United States, Singapore and the United Kingdom, where it has become dominant in some regions.
Researchers have since identified three subtypes, known as B.1.617.1 (the ‘original’ B.1.617), B.1.617.2 and B.1.617.3, each with a slightly different genetic make-up.
They are now rushing to investigate these variants and work out how they might affect the trajectory of the pandemic in countries where they have gained a foothold. Key questions remain about how quickly the variants can spread, their potential to evade immunity and whether they cause more severe disease.
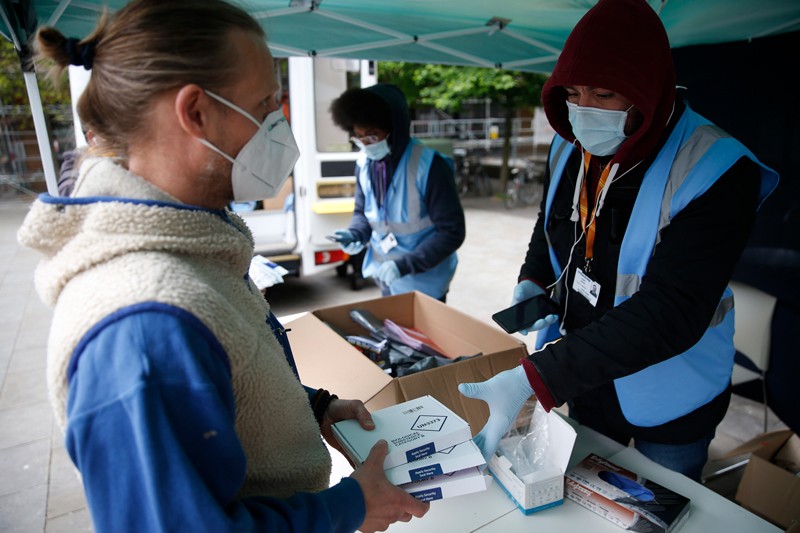
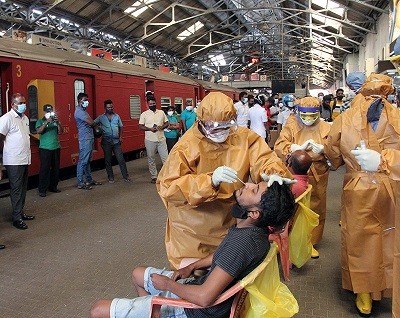
A lot of this research takes the form of standard epidemiology — confirming COVID-19 cases through testing, identifying the variants responsible for infections and cross-referencing these data to people’s clinical symptoms and vaccination statuses. Scientists can also glean insights from genomic-sequencing data, identifying which mutations are present in the B.1.617 subtypes and comparing these with mutations in earlier variants whose behaviour is better understood.
More transmissible
“I look at individual mutations because they each have individual properties that we think might confer higher transmissibility,” says Julian Tang, a consultant virologist at the Leicester Royal Infirmary, UK. Increased transmissibility — a measure of how quickly variants can spread from person to person — could accelerate outbreaks, which could put more pressure on health-care systems and counter-measures such as vaccination programmes. For example, the B.1.617.2 variant has mutations called 452R and 478K, which Tang says are both linked to increased transmissibility. Both mutations alter the spike protein, which the virus uses to enter human cells.
Researchers have also been able to rapidly track the spread of B.1.617.2 because its genome contains a marker that the dominant B.1.1.7 variant lacks. The presence of this marker — known as the ‘S gene target’ — can be seen in the results of some of the PCR tests used to confirm cases of COVID-19, so researchers can use positive S-target hits as a proxy to quickly map the spread of B.1.617.2, without needing to sequence samples fully. Both S-gene tests and more detailed sequencing data from UK virus samples indicate that B.1.617.2 is outcompeting the two other B.1.617 subtypes, and replacing B.1.1.7 — a variant identified in southeast England in late 2020 — as the most common variant driving new infections in the country.
“Across all of England now, we would expect that 50% of infections would be the [B.1.617.2] variant,” says Tom Wenseleers, a biologist at the Catholic University of Leuven in Belgium who is tracking the figures. An analysis of UK sequencing data that he shared online suggests that numbers of B.1.617.2 infections could be growing 13% faster than B.1.1.7 infections each day.
In a report published on 12 May, A UK government advisory committee called the Scientific Pandemic Influenza Group on Modelling, Operational subgroup said there is a “realistic possibility” that B.1.617.2 is 50% more transmissible than B.1.1.7, according to the available data.
“The prediction of 50% more transmissible sounds entirely plausible,” says Sharon Peacock, a microbiologist at the University of Cambridge, UK, who leads the COVID-19 Genomics UK consortium. “I think as data goes up more, we’ll get more confidence in that, but you can’t really ignore what’s happening.”
At present, Peacock adds, the surge in B.1.617.2 is not leading to a significant rise in the overall number of cases in the United Kingdom, which remain much lower than during the country’s most recent peak, in January. Instead, people are catching the new variant rather than B.1.1.7. “What we’re seeing here is lineage replacement,” she says.
Immune escape
Another question researchers are keen to resolve is whether vaccines will remain effective against the B.1.617 variants. If any of these strains can evade the immune protection conferred by vaccination, or by previous exposure to the virus, they could trigger significant new waves of infection and derail plans to relax lockdowns and other restrictions.
In theory, the accelerated spread of B.1.617.2 in the United Kingdom — where more than 50% of the population has received at least one dose of a COVID-19 vaccine — could indicate an ability to escape vaccine protection. But Wenseleers says there is little evidence that vaccine escape is driving the increase in cases. Preliminary data from Bolton, an outbreak hotspot in northwest England, from mid-May showed that most people there who were hospitalized with COVID-19 caused by B.1.617.2 had not been vaccinated. Some 5 out of 18 hospitalized people testing positive for the variant had received a single vaccine dose, and just one had been given both doses.
Separate data analysed by Wenseleers showed that infections with the B.1.617.2 variant in northwest England were initially clustered in teenagers, who are not routinely vaccinated. Although the variant subsequently spread to people in their thirties and forties, those in their fifties — who are more likely to have had both vaccine doses — experienced lower rates of infection. “That is reassuring,” he says.
Genetic-sequencing data suggest that the rapid spread of B.1.617.2 is less likely to pose a problem to vaccination efforts than spread of B.1.617.1. The 452R and 478K mutations identified in B.1.617.2 are both linked to vaccine escape as well as increased transmissibility, says Tang. But B.1.617.1 also carries a different mutation called 484Q, which is more strongly associated with vaccine escape1. This mutation isn’t found in B.1.617.2.
Reassuringly, no mutation in any of the B.1.617 variant subtypes is associated with increased disease severity, Tang says.
Researchers can also conduct laboratory tests to check how well antibodies neutralize different viral variants. A study published on 17 May in Nature Medicine2 suggests that such tests are “highly predictive” of real-world immune protection. Some of these lab studies indicate that vaccines could be less effective against the B.1.617.1 subtype1. Results from similar experiments with B.1.617.2 have not yet been published, but data released by Public Health England on 23 May suggest that the Pfizer-BioNTech and Oxford-AstraZeneca vaccines are effective against B.1.617.2 after two doses.
Modelling future spread
Some key uncertainties remain, including how much more transmissible B.1.617.2 is than other variants, such as the B.1.1.7 variant now established in the United Kingdom and many other countries. “It’s plausible that it could be 50% greater, but it could also be 10% greater, or 60–70% greater,” says Christina Pagel, a health-care researcher at University College London. Establishing this will allow scientists to build more accurate models of the effects the variants could have on outbreaks in countries where they are becoming dominant, including the United Kingdom. “It makes a massive difference in terms of what will happen in the summer,” says Pagel. “The difference from 20% to 50% is like the difference between a moderate wave and a January-style surge. So that really needs pinning down.”
Pagel also questions whether the results on vaccine effectiveness are reassuring. “Saying the vaccine is ‘effective’ isn’t very helpful, because there’s a range of effectiveness,” she says. Vaccine-efficacy studies tend to focus on the ability to prevent severe disease and death. But it’s also important to know whether vaccinated people could catch the B.1.617.2 variant without getting ill, and pass it on, she says. If that is the case, “you don’t get the same level of population immunity than you would otherwise”.
Peacock says continuing to gather epidemiological data from the UK outbreak will help to answer those questions. It will also help to forecast the potential impact of B.1.617 variants in other countries, particularly developing nations, which do not yet have widespread access to vaccines. “It’s important that we provide a service to the world by making those measurements,” she says.
What scientists know about new, fast-spreading coronavirus variants - Nature.com
Read More



No comments:
Post a Comment